What is CPR?
Cardiopulmonary resuscitation (CPR) is a lifesaving technique useful in many emergencies, including heart attack or near drowning, in which someone’s breathing or heartbeat has stopped.
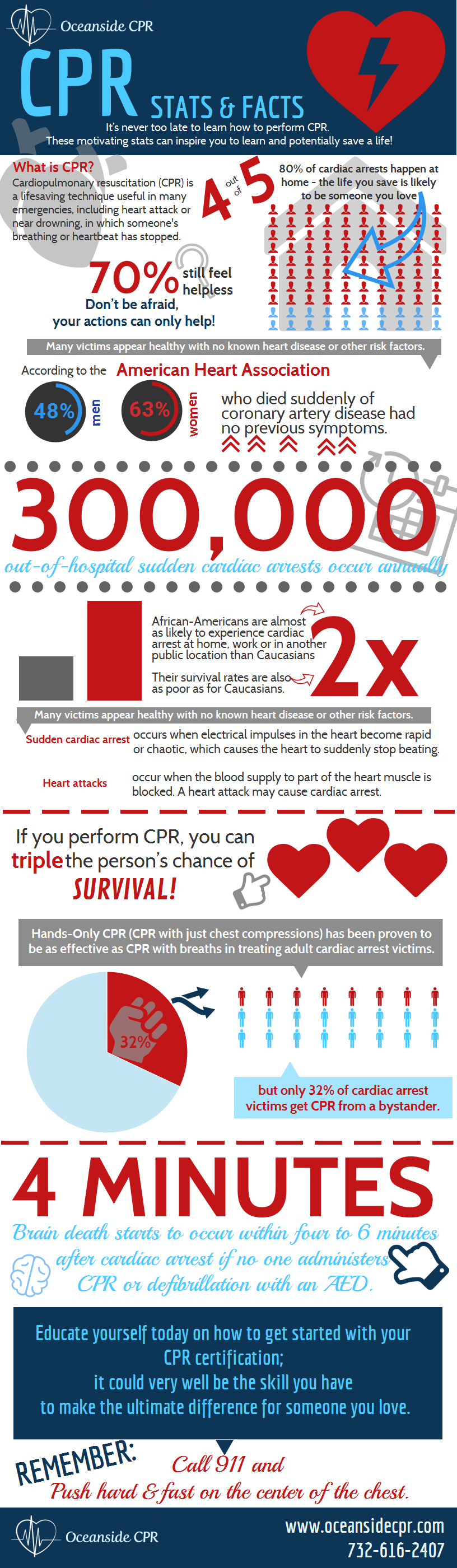
CPR Stats and Facts
Seventy percent of Americans feel helpless -to act during a cardiac emergency because they either do not know how to administer CPR or their training has significantly lapsed. Educate yourself today on how to get started with your CPR certification; it could very well be the skill you have to make the ultimate difference to someone you love. Take a look at these stats and then give us a call:
Share This Infographic On Your Site
- Nearly 300,000 out-of-hospital sudden cardiac arrests occur annually
- Many victims appear healthy with no known heart disease or other risk factors.
- African-Americans are almost twice as likely to experience cardiac arrest at home, work or in another public location than Caucasians, and their survival rates are twice as poor as for Caucasians.
- Sudden cardiac arrest is not the same as a heart attack.
- Sudden cardiac arrest occurs when electrical impulses in the heart become rapid or chaotic, which causes the heart to suddenly stop beating.
- A heart attack occurs when the blood supply to part of the heart muscle is blocked. A heart attack may cause cardiac arrest.
- Effective bystander CPR provided immediately after sudden cardiac arrest can double or triple a victim’s chance of survival
- If you perform CPR, you can triple the person’s chance of survival
- but only 32% of cardiac arrest victims get CPR from a bystander.
- Hands-Only CPR (CPR with just chest compressions) has been proven to be as effective as CPR with breaths in treating adult cardiac arrest victims.
- Brain death starts to occur within four to 6 minutes after cardiac arrest if no one administers CPR or defibrillation with an AED does not occur during that time.
- Less than 8% of people who suffer cardiac arrest outside the hospital survive.
Don’t be afraid, your actions can only help!
If you see an unresponsive adult who is not breathing or not breathing normally, call 911 and push hard and fast on the center of the chest. Anyone can learn CPR – and everyone should!
CPR AED Training Classes At Oceanside CPR
Consider taking a CPR AED training class at Oceanside CPR . Our program is an excellent choice for both the community and workplace and teaches skills with research-proven Practice-While-Watching (PWW) technique, which allows instructors to observe the students, provide feedback and guide the students’ learning of skills.
As CPR instructors with over 25 years of experience, we are able to provide a relaxed and comfortable teaching environment, no matter what class you are looking for. Our goal is to prepare people with the confidence so they can perform CPR in any life-threatening emergency – Without Hesitation! Whether you are interested in attending a class, scheduling an on-site training or just have a general question, please don’t hesitate to contact us at (732) 616-2407.
]]>CPR, or cardiopulmonary resuscitation, is a procedure that will save an individual’s life if they have stopped breathing or their heart has stopped beating. This is usually the result of choking, drowning, suffocation, or other medical issues such as cardiac arrest. CPR is a combo of providing oxygen to the lungs through rescue breathing and keeping the blood flowing by providing chest compressions.
If blood flow does stop, permanent brain damage or even death can happen within just a few minutes. Therefore, response time is critical. An individual can be easily trained in proper CPR procedures through a corporate onsite CPR training course.
Things to Consider
While it’s true that CPR is a lifesaving procedure, it’s best if performed by someone who has been trained. If you have not been trained, consider trying to find a corporate onsite CPR training course to help you learn, especially if you are a parent or someone who cares for children and infants on a regular basis.
The American Heart Association is currently teaching the new technique of emphasizing the importance of chest compressions over rescue breathing. You can still learn the traditional technique if you wish in a corporate onsite CPR training course.
What Causes an Infant’s Heart to Stop?
There are many different things that can cause an infant’s breathing and heartbeat to stop. These include: head trauma, poisoning, choking, electrical shock, suffocation, drowning, and more.
When Should CPR be Performed on an Infant?
If an infant is not breathing, has no pulse, and is unconscious, then CPR should be performed.
Things to Avoid
There are certain things that you should do and certain things you should not. These would be covered in depth in a corporate onsite CPR training program.
If an infant is unconscious, you should never shake them to try to get a response. Pinching them is the best way to try to see if they are okay.
When performing CPR on an infant, you should never lift their chin while tilting the head back to move the tongue from the airway. If you suspect a spinal injury, you should simply pull the jaw forward without disturbing the neck or head. Never allow the mouth to close.
If the infant is breathing normally, moving, or coughing, you should not begin chest compressions because that could result in the heart stopping.
When to Call for Emergency Medical Help
If there is someone else there with you, one of you should call for emergency medical help while the other one begins CPR procedures. However, if you’re alone, loudly call for help and then begin lifesaving procedures. After two minutes, if no help has arrived, you should call for emergency medical response.
As long as you don’t suspect a spinal injury, you can carry the infant with you to a phone if you need to.
Preventing Accidents
In most cases, the incident causing the need for infant CPR is a preventable one. Following are some tips that can help prevent you from needing infant or child CPR.
- Assume an infant is more capable than you think. They can move around much more than you may want to give them credit for.
- You should never leave infants unattended on a surface that they could roll or fall off of.
- When putting a child in a high chair or stroller, always strap them in. You should never leave a child in a playpen with one of the sides down, and always follow precautions when using a car seat.
- You should teach your baby early on the meaning of “no” and “don’t touch.”
- Store toxic cleaning solutions and other chemicals in a childproof cabinet so that children can’t get their hands on them.
- Make sure that the environment is safe for children and infants.
- Always sit with an infant when they are eating – never allow them to move around while eating or drinking.
- Never tie anything around an infant’s wrists or neck.
Sources:
http://www.nlm.nih.gov/medlineplus/ency/article/000011.htm
]]>
In most cases, taking part in a corporate onsite CPR training class will also include first aid. These types of classes are wonderful because they can teach an individual what to do in case of an emergency. CPR, or cardiopulmonary resuscitation, is wonderful because you can use it to prevent the victim from suffering brain damage or dying.
What is Basic First Aid?
The term “basic first aid” means the process of first assessing the needs and situation and then addressing those needs of an individual who has been hurt or is in some sort of physiological distress. First aid courses, including corporate onsite CPR training, will help you to easily and quickly determine the physical condition of the individual and then to figure out the best course of treatment. Of course, the help of a medical professional should be sought as soon as possible, but there are some things that you can do to make the difference between life and death for the victim.
What are the Steps for Basic First Aid?
There are four steps that you will need to follow in order to perform first aid. These things would be addressed further in a corporate onsite CPR training course, but this is a great introduction. First, you will need to assess the situation and the victim – this includes calling for help. Then, you will begin caring for the victim. Finally, you should be aware of the various scenarios that could take place – there are some fairly common things that could have happened to the victim; then there are some rarer ones.
Getting Started with Basic First Aid
If you witness a victim in distress, you will need to start with the three C’s of first aid. While it’s true that your priority is helping this victim, you also have a right to make sure that you are protected and safe. This means that before rushing into an emergency situation to help someone, you should take a moment to evaluate the situation and surroundings. Pay attention to whether there are things that could possibly cause you harm. After all, you don’t want to rush into a situation where you will end up just like the person you’re trying to help.
If there are things that could endanger your life, you immediately get professional help. Medical professionals, such as paramedics, have much higher levels of training. Basic first aid, such as that learned in a corporate onsite CPR training course, will become completely useless if you end up hurting yourself.
After assessing the situation, you’re going to need to call for help. If you feel like the individual is seriously injured, you should call for help immediately. On the other hand, if you’re the only one on the scene, and the victim is not breathing, attempt to establish breathing again before calling for help. You should make sure that you never leave the victim alone for an extended period of time.
Finally, now that professional medical help is on the way, you can begin using your first aid training that you learned in your corporate onsite CPR training course to treat the victim. Keep in mind that taking care of a victim that has just experienced a serious trauma will include both emotional support and physical treatment.
One of the most important things to do is to keep yourself calm and try to reassure the victim. Let them know that you do have help on the way and everything is going to be okay. Remember, taking a corporate onsite CPR training class will be the best way to learn both CPR and first aid.
Sources:
http://www.wikihow.com/Do-Basic-First-Aid
]]>There are many different situations when CPR can potentially save a person’s life or minimize brain damage and other health problems. Though use of CPR is not always enough to guarantee a person’s survival, when used correctly, it can dramatically increase their chances. CPR training in NJ can help you learn how to identify these life-threatening situations and how to immediately respond. With CPR training in NJ, you’ll have to tools to potentially save the life of a friend, coworker, family member, or stranger.
Situations to Use CPR
When you see someone unconscious or collapsed on the ground, they may need CPR and other forms of assistance. CPR, also known as cardio pulmonary resuscitation, can help restore breathing and beating of the person’s heart and save their life. Individuals who complete AED and CPR training in NJ are better prepared to identify people who might need this type of help.
Some situations that may require CPR include drowning, suffocation, heart attack, allergic reaction, choking, and electric shock. One of the most common situations when CPR is needed is during sudden cardiac arrest. This occurs when a person’s heart suddenly stops beating. This is why it’s so important to check breathing and heartbeat when you encounter someone who looks unconscious.
Cardiac arrest typically happens after a person experiences an especially long or severe type of heart arrhythmia, which is when the heart beats in an irregular rhythm or too slowly or quickly. Anyone could have minor cases of arrhythmia, but some people experience arrhythmia more often or have more serious cases of arrhythmia, and this makes sudden cardiac arrest more likely. Some common causes of arrhythmia include:
Coronary Heart Disease
If you have coronary heart disease, your arteries slowly clog with cholesterol and other deposits. This reduces the amount of blood that can flow to your heart and affects the ability of your heart to beat at a proper rhythm.
Heart Attack
During a heart attack, a person may experience ventricular fibrillation, which is when the lower chambers of the heart wither but do not contract effectively. This is one of the most common causes of heart attacks and one of the most common reasons why people need CPR or AED. CPR training in NJ can teach you how to recognize when this is happening and help you provide treatment quickly and correctly.
Congenital Heart Disease
Some people are born with abnormalities in their heart, and this can make the risk of heart attack and arrhythmia higher. This can even affect adolescents and children and cause them to experience sudden cardiac arrest. When providing CPR to younger victims, it’s very important that the person understand what they are doing. Courses that provide CPR training in NJ teach participants how to provide CPR to different ages, so that you are always prepared during an emergency.
Problems With the Electrical System
Every person’s heart is controlled by electrical signals. These electrical signals tell the heart when to contract, how fast to contract, and how much to contract. When the electrical system is working correctly, the heart beats a normal rhythm, but sometimes the electrical systems stops working the way it’s supposed to. These types of problems are known as primary heart abnormalities. Though rare, there are some conditions that can cause these types of abnormalities such as long QT syndrome and Brugada’s syndrome.
These are only a few of the possible causes of arrhythmia and sudden cardiac arrest. There are many different reasons why a person may suddenly require medical attention, and that’s why CPR training in NJ is so important. Contact us to learn more about our programs and services.
Sources:
http://www.mayoclinic.org/diseases-conditions/sudden-cardiac-arrest/basics/causes/con-20042982
]]>After a person completes corporate onsite CPR training, they’ll be prepared to respond in a number of different emergency situations. If someone collapses, they will be able to apply their training and respond appropriately. They’ll even be trained to use the AED, the automated external defibrillator, to provide electrical stimulation to the heart and help the heartbeat at a normal rhythm. Some of the reasons why someone may need CPR include choking, suffocating, electric shock, severe allergic reaction, and drowning.
Though there are a variety of reasons why a person may require CPR, two of the most common reasons are heart attack and sudden cardiac arrest. These two conditions are related, but they are not the same. Unfortunately, if you don’t have a medical background, it is likely that you don’t know the difference between a heart attack and sudden cardiac arrest.
Understanding the difference is important because it can help you respond more effectively during an emergency. It can also help you communicate more accurately over the phone and with medical professionals who arrive on the scene, and this can save precious seconds when they work to revive the victim. Corporate onsite CPR training can be a great way to teach coworkers more about heart attacks and sudden cardiac arrest and give them the tools to respond correctly in these life-or-death situations.
What Is a Heart Attack?
There is a lot of confusion among the general population about what is and isn’t a heart attack. A heart attack is caused when the blood flowing to a section of the heart is reduced or stopped completely due to blockage in an artery. Though heart attacks can be acute and happen suddenly, they are often more gradual. The artery becomes significantly clogged, and the reduced blood flow causes a part of the heart to get weaker and weaker until the symptoms become very severe.
During many heart attacks, the heart continues to beat, but not enough blood is reaching the heart. However, sometimes the person goes into sudden cardiac arrest. Individuals with corporate onsite CPR training may be able to provide CPR and use an AED to help the heart start beating normally.
What Is Sudden Cardiac Arrest?
Sudden cardiac arrest is when a person’s heart suddenly stops beating. There are many different reasons for sudden cardiac arrest, but it typically is related to the electrical signals that control the rhythm of the heart. If a person’s heart begins to beat too quickly, too slowly, or at an irregular rhythm, this can lead to sudden cardiac arrest. Corporate onsite CPR training can help teach employees how to check for a person’s heartbeat and identify if sudden cardiac arrest has occurred.
Though heart attacks and decreased blood flow can affect the ability of the heart to beat at a healthy rhythm, these two conditions are not always related. Sometimes a heart attack is not followed by sudden cardiac arrest, and sometimes sudden cardiac arrest occurs even though the person never had a heart attack.
Whether it’s a heart attack or sudden cardiac arrest, it’s important that the person get medical attention immediately. Coworkers should call 911 as soon as possible. If the person stops breathing or if their heart stops beating, it is very important that someone begins CPR and finds a nearby AED. Corporate onsite CPR training can be crucial in these situations. AEDs are especially important during sudden cardiac arrest, as they can restart the heart and prevent further damage or death. If you’d like to learn more about how we can provide corporate onsite CPR training to your company, contact us today.
Sources:
]]>Today CPR is one of the most accepted and standardized techniques used by emergency responders, and corporate onsite CPR training is offered in almost every major company and business in the United States. Though this has been the case for decades, there was a time when the technique was less accepted by the public and the medical community.
Like other medical breakthroughs, CPR was not discovered all at once. Instead it was slowly studied and refined until it became the standardized life-saving procedure that it is today. From its beginnings in the 1700s, cardiopulmonary resuscitation has continued to evolve as doctors have learned more about the human body, and now it is an extremely effective way to provide emergency medical response to a person suffering from sudden cardiac arrest.
The Beginning
The first mentions of the procedures that would one day become CPR appeared in the middle of 18th century. The Paris Academy of Science began to endorse mouth-to-mouth resuscitation for drowning victims in 1740.
Around the same time, the Society for the Recovery of Drowned Persons was organized. This organizations was founded in Amsterdam in response to the hundreds of citizens who died by drowning in the canals every year. Though not all of the society’s ideas were medically accurate or effective, some of their practices were very similar to how CPR is performed today. These practices would spread to other organizations that provided medical assistance to drowning victims, but it would still be some time before doctors and others studied these techniques in detail.
In the next 150 years, the medical community learned more about the human body and began to study resuscitation. Finally at the end of the nineteenth century two doctors, Dr. Friedrich Maass and Dr. George Crile, independently documented the medical use of chest compressions to resuscitate someone who had drowned. Dr. Maass performed and documented chest compressions, and Dr. Crile had similar success in 1903. From then on, medical organizations adopted chest compressions as a way to revive those who had drowned.
Mouth-to-Mouth CPR
Then in the 1950s, there was another breakthrough in cardiopulmonary resuscitation research. Dr. Peter Safar, Dr. James Elam, and Dr. Archer Gordon were able to prove that mouth-to-mouth resuscitation could provide adequate oxygen to the body and increase the chance of survival of a drowning victim. In 1956, they developed techniques that made mouth-to-mouth CPR more effective, and soon these practices were adopted by the U.S. military and emergency medical services.
In 1960, the American Heart Association started to teach physicians how to perform CPR. In the next decades, the practice became more and more accepted. The first large scale CPR training occurred in Seattle, Washington in 1972. Leonard Cobb led the training program called “Medic 2” which trained more than 100,000 people in the program’s first two years.
CPR in Businesses
Businesses also started providing corporate onsite CPR training, so employees could perform the technique during an emergency, and this became more and more common. Corporate onsite CPR training is now found in many of the world’s largest corporations and businesses. Not only does it help make offices safer, but it’s also a great team-building and leadership opportunity for organizations.
If you are interested in corporate onsite CPR training, there are many ways that you can provide training on a flexible schedule and give participants the chance to get certified in CPR. Our corporate onsite CPR training programs are designed to make CPR approachable and easy to learn, so that your staff will be able to use these techniques to save the lives of coworkers, family members, and anyone else who needs help.
Sources:
]]> It’s Alive!
It’s Alive!
We’re pleased to announce that our new website is now live; it has been completely revamped and refreshed with each of our user’s needs in mind. We have redesigned our layout and navigation so you can easily find information and quickly register for CPR classes. The menus and registration process have both been enhanced and completely simplified.
Modern Look
You’ll notice that our new website has a modern, sleek look featuring a fresh layout to make it easier for you to find a CPR, AED and BLS class to fit your schedule. Plus, since it’s mobile-friendly, you can access it on the go and conveniently book your class right from your phone or tablet.
Find What You Need
We’ve put added focus on the on-site group classes including CPR, BLS, first aid training and certification options for larger groups. Plus you can now conveniently filter your search by date, location and subject.
Personalized
Our mission is to spread awareness of the importance of CPR and BLS skills and we’re excited to share this easy-to-use site with visitors. As CPR instructors with over 25 years of experience, we are able to provide a relaxed and comfortable teaching environment, no matter what class you are looking for. Our goal is to prepare you with the confidence so you can perform CPR in any life-threatening emergency – Without Hesitation!
Enrich Knowledge
Our sleek new design makes it easier to access our blog, learning about qualities of a good CPR instructor, how to choose a CPR training class, FAQs regarding CPR classes and important updates in the news.
Get Connected
Stay in the know through our social media channel buttons linked conveniently in the bottom right of the website to foster improved communications about the importance of CPR on Facebook, Twitter and Google+.
We, at Oceanside CPR, hope you enjoy the fresh look of our new website, designed specifically with each of your needs in mind. We look forward to hearing your feedback and feel free to contact us if you have any questions.
]]>As you’ll read in multiple other sections of this supplement, we continue to discern insights into more effective treatment approaches to out-of-hospital sudden cardiac arrest. In reality, we’ve collectively learned more in just the last decade than ever before about the pathophysiology of cardiac arrest.
With considerations about cooling (therapeutic hypothermia), chest compression continuity and alternative ventilation strategies, is there really much to talk about when it comes to something as simple as the rate of chest compressions?
“So, Dr. G, what’s your interest in chest compression rate? The American Heart Association (AHA) says to compress the cardiac arrest victim’s chest at least 100 times a minute. That’s all there is to it, right?”
That’s a good place to start and an understandable question. For purposes of this particular conversation, let’s discuss victims who are of adult age. You’re correct in your interpretation of the AHA guidelines released in late 2010.1 How the 2015 guidelines on chest compression rate will change, if at all, is unknown.
There’s been some interesting science published regarding chest compression rates since those 2010 guidelines.2,3 I’m quite sure the clinicians and scientists charged with formulating those 2015 guidelines will certainly take such discoveries into account. The fact is — no surprise here, I think — nothing is very simple when it comes to a condition as dynamic, dramatic and challenging as cardiac arrest.
Key among the latest scientific papers on chest compression rate is work done by Dr. Ahamed Idris and his colleagues in the Resuscitation Outcomes Consortium. In short, Dr. Idris and the research team found that exactly 100 chest compressions per minute didn’t produce the highest number of survivors among the large group of cardiac arrest victims who were treated by systems that participate in the ROC.4
The “sweet spot” of chest compression rate in that review, published in 2012, was much nearer to 120 chest compressions per minute.4 So, you might say that the AHA is still right because 120 compressions per minute fits the definition of “at least 100 times a minute,” although so does 140 compressions per minute, correct?
“The patients (and their families) we treat often think more is better, and if we want to be honest, many EMTs and paramedics subscribe to that belief about a lot of interventions. That said, I bet you’re getting ready to burst that bubble and tell us 140 compressions per minute may not be better?”
Actually, I’m not going to say 140 compressions per minute may not be better than a rate of 120. Instead, I’m going to say, based upon the Idris paper, that 140 compressions per minute are definitely not better for survival than 120. In that report, a very compelling graph is presented that I choose to describe as a “wave of survival per compression rates.”
The reason I call it a “wave” is that a curve implies an even rise and fall and this isn’t that. The scientific term for the actual curvilinear shape is a cubic spline model, but that’s hard for a guy like me to immediately grasp. I can visualize a wave that rises and then fades out, and I think most people can as well.
So back to that study, it’s not too hard to imagine that survival proved lower at rates less than 100 compressions per minute and then there is a slow increase to a peak in survival near 120 compressions per minute.
Here’s my key point: After 125 and towards 140 and beyond, the survival line drops off! That’s why this study is so important in my opinion, and I trust the researchers, their method of study, plus the number of patients involved was large. This is science you and I can use in our quest to produce more neurologically intact survivors from out of hospital sudden cardiac arrest.
“Why do you think 140 isn’t better than 120? Besides, are people in real life compressing at 140 anyway? That seems pretty fast and not what’s taught in the first place.”
Let me break that up into two answers. First, we have to think about this amazing organism that is the human body. What happens when you and I decide we’re going to get our particular organisms in better shape and do some aerobic conditioning or weightlifting? Why does our heart rate rise and breathing increase? We are doing the “Magic C” as I call it — compensating!
That workout-induced tachycardia and tachypnea is getting greater-than-usual oxygen-enriched blood flow to muscles that require it to perform what we’re asking of them. As long as we are pulsatile, and your patient is pulsatile, our human bodies will stretch compensation to impressive levels. But, what happens when pulsatile becomes pulseless? Compensation ceases, at least the intrinsic compensation.
So what’s the extrinsic compensation during CPR? You. Me. Your partner(s). Bystander(s). CPR is, in one word, compensation.
What percent of compensation do you and I have to attain for a person when we do CPR? 100%! Sobering, huh? We don’t even get to outsource 1%; that 100% needs to be the very best it can be, at least according to the best understanding of what works today.
As important as each compression is, the decompression phase is just as important because that’s when intrathoracic pressure drops and blood flow can return to the heart to be available for flow from the heart on the next compression. Think about the last sick patient you had in a true tachydysrhythmia with a pulse? Why were they so weak, hypotensive and likely even hypoxic? The rapidity of their pulse prevented good cardiac output and perfusion, both to central and peripheral circulation.
We may not be so worried about peripheral perfusion in cardiac arrest, but if our compressions are going to produce helpful cerebral and coronary perfusion pressures, we have to let enough decompression time occur. That doesn’t happen if we compress at 140 times a minute.
So do professionally trained EMTs and paramedics compress that fast anyway? Actually, yes, a lot do. Good – hearted, enthusiastic police officers, firefighters, EMTs and paramedics perform too many compressions. How do I know this? Back in 2011, we discovered in the process of reviewing chest compression fundamentals with each and every EMT and paramedic in the EMS System for Metropolitan Oklahoma City and Tulsa, that without a metronome to guide compressions, nearly 90% of these incredibly well-trained men and women were compressing somewhere between 135–145 times per minute!
That really opened my eyes. It affirmed to me several things: 1) We have EMS professionals in our system who really care about — and work hard at — treating cardiac arrest. Even in training scenarios, their adrenaline kicks in and they go after it! I had honestly thought if we did start using metronomes set at 120 beeps per minute, directly influenced by that ROC study we’ve been talking about, those metronomes would be needed to speed up the rates. But, I was wrong. The reverse was true; we were compressing too fast and the metronomes would help us to slow down.
It became crystal clear to me we needed to begin using metronomes to change natural compression rate tendencies. This turned out to not just be a positive for the patients, but our crews also, because we were actually able to reduce the physical work necessary in performing optimal manual chest compressions.
“Cool, Dr. G. So just compress at 120 a minute in adults, use metronomes set to that and that’s all there is to it?”
Even with what we’ve discussed so far, there’s more to it. To prove the point, I’ll share with you now that we recently changed our compression rate guideline, and metronomes, to 110 compressions per minute in rate.
“What?!?! How does that make sense based upon what we’ve been talking about?”
Back to the “nothing is really simple when it comes to cardiac arrest” mindset. In our particular system, we currently don’t use mechanical chest compression devices like the Physio-Control LUCAS 2 chest compression system or ZOLL AutoPulse non-invasive cardiac support pump. We use a team dynamic plan for coordinated resuscitation (aka the “pit crew” approach). The most common resuscitation in metro Oklahoma City or Tulsa has 5–8 EMS professionals on scene within 4–10 minutes.
In addition, one of the devices we choose to use in our airway management and cardiac arrest care is the ResQPOD impedance threshold device (ITD) for its capability of reducing intrathoracic pressure during decompression — another important factor in cardiac arrest resuscitation.
Further, because of the emphasis we’ve been placing on the continuity of chest compressions and getting quick feedback to our colleagues about how consistent in rates and continuity that their compressions were or were not in individual resuscitations, we’ve seen our chest compression fraction (time of resuscitation in which chest compressions are occurring) move from a typical 85% to more than 95%.
Without getting too far down in the weeds of science, it’s important to point out that use of mechanical chest compressors and/or the impedance threshold device can influence the basic physiology of hemodynamics produced by compressions.
Through very in-depth conversations that I’ve had over the past few years with the clinical scientists who developed the impedance threshold device, it appears that the ideal compression rate for CPR without an ITD, as reported in the Idris paper, differs from what’s ideal if an impedance threshold device is used in-line in the airway circuit.
It seems the best rate when using an impedance threshold device is much closer to the 100 compression rate per minute; in fact, in subsequent data analysis, the best overall survival in the ROC study occurred in patients who received an active ITD with chest compression rates close to 100/min. So, we’re slowing down to 110 for now, primarily based upon both this specific data analysis and our system-specific chest compression fraction and effective compressions per minute. We’ll continue to follow our survival outcomes and adjust our chest compressions rates as further observation and science dictates.
To illustrate how complex this can get, if active compression – decompression CPR with an ITD finds its way to the streets of the United States, that ideal chest compression rate may be as low as 80/min according to a recent U.S. study!
It does make sense when you appreciate that all of these things produce different compression types and intrathoracic pressure and, thus, different compression types and adjuncts, like the ResQPOD ITD and mechanical compression devices, will produce different optimal rates.
Just remember, it still is all about survival and there are a lot of “fine tuning” knobs to turn back and forth as science gives us updates to our user’s manual for resuscitation.
“Wait, Dr. G. So you’re talking a lot about rate, but not so much specifically about metronomes. Seems like those are more important than you first thought and if anything, they’re getting even more important. Why don’t the monitor/defibrillators have metronomes adjustable from 100 per minute? Should we ignore those? And, what metronomes should we be buying?”
First, you’re right. Metronomes are far more important than I first thought. In fact, credit goes to paramedics in our system who pushed the concept. I’ll claim to be smart — smart enough to listen to what proved to be their great idea.
Those early metronomes came about because not all the responding companies (fire-based) had manual monitor/defibrillators and not all of our monitor/defibrillators had built-in metronomes at the time. And, for my manufacturing colleagues reading this article, I’ll admit some frustration at the lack of their built-in metronomes being changeable in rate. But, I’ll also admit that I understand the frustration that these manufacturers have themselves because they can’t put a “dial the rate up or down” knob or touchscreen on their devices without a time-intensive and costly journey through the Food and Drug Administration review and approval process.
Should you ignore those metronomes that come with the cardiac monitor/defibrillators? Not if your local medical oversight physician(s) want you to use them. If they do, please use them per your system-specific treatment guidelines.
In our system, we’ve purchased musical metronomes that do allow for rate changes. This made it possible to start at 120 beeps per minute, change to our current 110 beeps per minute, and still allow for future changes. I’m pretty sure these music industry companies have no idea what paramedics are doing ordering dozens of metronomes. They probably think we’ve got some great garage bands in urban Oklahoma!
Many options exist in the marketplace. I recommend you try to find something that’s easy to activate and see or hear, with the durability of the proverbial EMS steel ball, something that allows for rate changes (but doesn’t allow crews to change it to undesired rates or allow unintended changes in rates), and something sized to promote ready accessibility.
There are a lot of smartphone apps with audible and visual metronomes that are adjustable as well. We considered use of smartphone apps, but didn’t want to ask our EMS professionals to use their personally owned devices in the provision of resuscitation.
Many of the agencies in our EMS system have found great ways to physically attach metronomes to the outside of their AEDs or manual monitor/defibrillators so initial arrival EMTs and paramedics don’t have to go fishing in a pocket or compartment to find it in the early and chaotic first minutes of resuscitation. Easy access always promotes consistency in early use.
“So, Dr. G.: What kind of improvement have you seen in resuscitation practices in the EMS System for Metropolitan Oklahoma City and Tulsa since your crews started using these metronomes during cardiac arrest resuscitations?”
We made an assumption when the pit crew protocol was finalized and initially implemented, that the medics were providing 120 compressions per minute per our protocol. All of the involved agencies had metronomes at that time and there was nothing to lead us to believe this rate was in question.
When we participated in a cardiac arrest resuscitation analytics annotation pilot project sponsored by one of our industry partners in February and March of 2014, we found that the compression rates on some cases were alarmingly high while others were at or near 120. So we added a field to the data we collect and the CPR rates have been continuously tracked since that time.
One of the things we found early on was that some of the smaller sized metronomes were not being used for various reasons. In some cases, it was simply because the crews forgot to use them, though in others it was because the Velcro that had been used to attach them to the monitors had become worn and the metronomes either fell off and were lost, or they were simply placed in the monitor case where EMTs and paramedics didn’t know they were relocated. Like they say, out of sight can equal out of mind!
We also learned that environmental noise can cover the sound of the metronome, so, whatever metronome you use, it has to be capable of being heard and/or seen. The metronomes built into the cardiac monitor/defibrillators do seem to solve that problem, but I want to caution that I personally don’t think 100 compressions per minute for all cardiac arrest patients, in all resuscitation practices is the optimal rate as we know it today.
In all of the cases in our specific system when the metronome wasn’t used, the compression rate was certainly faster than the 120/min we desired. Interestingly, when the ambulance would go en route to the hospital, rates often jumped almost immediately from around 120 to 130 and above.
After we mounted a concerted effort to have the providers utilize the metronomes and began revealing the patterns in compression rates at our monthly CQI meetings and additionally in emails to the education departments in our system agencies, we found almost immediate elimination of extreme compression rate deviations (e.g., greater than 160/min).
Our typical rate is now 123/min. Keep in mind we’re still rolling out the change to 110/min. This is down from 129/min. It doesn’t sound like much, but there are nearly 100 workable arrests every month in our system and that’s a great achievement by our fire and EMS crews in focusing on hitting that compression “sweet spot” of compressions per minute. We believe it has strongly contributed in increasing our successful resuscitations.
“Thanks, Dr. G. Do you have any parting thoughts?”
It’s an exciting time in EMS resuscitation. It takes work on everyone’s part to keep pace with the findings we’re putting into practice. Thanks for your commitment to excellence in out-of-hospital EMS medicine by reading this article. Together we’re finding better answers to challenges like cardiac arrest, answers that truly make a life or death difference to people we serve, and when they need those answers most. Keep reading and asking questions because scientific discoveries are happening in EMS medicine now more than ever.
References
1. Field JM, Hazinski MF, Sayre MR, et al. Part 1: Executive summary: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(suppl 3):S640–S656.
2. Field RA, Soar J, Davies RP, et al. The impact of chest compression rates on quality of chest compressions: A manikin study. Resuscitation. 2012;83(3):360–364.
3. Jäntti H, Silfvast T, Turpeinen A, et al. Influence of chest compression rate guidance on the quality of cardiopulmonary resuscitation performed on manikins. Resuscitation. 2009;80(4):453–457.
4. Idris AH, Guffey D, Aufderheide TP, et al. The relationship between chest compression rates and outcomes from cardiac arrest. Circulation. 2012; 125(24):3004–3012.
5. Aufderheide TP, Nichol G, Rea TD, et al. A trial of an impedance threshold device in out-of-hospital cardiac arrest. N Engl J Med. 2011;365(9):798–806.
6. Aufderheide TP, Frascone RJ, Wayne MA, et al. Standard cardiopulmonary resuscitation versus active compression-decompression cardiopulmonary resuscitation with augmentation of negative intrathoracic pressure for out-of-hospital cardiac arrest: A randomized trial. Lancet. 2011;377(9762):271–352.
7. Kern KB, Stickney RE, Gallison L, et al. Metronome improves compression and ventilation rates during CPR on a manikin in a randomized trial. Resuscitation. 2010;81(2):206–210.
Las Vegas firefighters are garnering increased attention for their hands-only CPR training. As one of the locales leading the way for cardiac arrest survival rates, Las Vegas is approaching incredible 25% survival numbers and even has its sights set on reaching 50%. The hands-only CPR approach is appealing to many who might have reservations about doing mouth-to-mouth resuscitation. The positive numbers do not, however, appear to reflect the element of chance; Las Vegas firefighters have made it their goal to increase CPR training and to improve people’s chance for survival.
Short and Simple
One of the hallmarks of the Las Vegas Firefighters’ program is that is easy. The hands-only technique is not overly difficult for people to learn. Moreover, the instruction can be achieved in a mere matter of minutes. The program is also free which makes it easier to promote to community residents. Many people are happy and even grateful to have the opportunity to learn the life-saving techniques so quickly and at no cost. The firefighters are hoping to bring their training to increasing numbers of people. So far their efforts have been rewarded with those increased survival rates.
Hands-Only CPR
Sometimes referred to as ‘compression-only’ CPR, this technique is gaining in popularity around the country but especially in urban areas. Hands-only can be a viable form of CPR, especially where emergency responses tend to be quick. In more remote places, compression and mouth-to-mouth CPR increases people’s chance for survival. The hands-only form of CPR can save a life and preserve good neurological (brain) function when properly conducted. The firefighters have also designed an app to accompany the training that users may refer to for information. According to the Las Vegas Review-Journal, the app “notifies those trained in the use of CPR and the operation of the Automatic External Defibrillator when they are within 200 yards of a cardiac emergency that has been called into the fire department.” The app can also tell people where the nearest public AED is in reference to the incident site. (reviewjournal.com/columns-blogs/john-l-smith/las-vegas-firefighters-lead-way-cpr-training)
Innovative Approaches to CPR Training
CPR is getting more attention throughout the U.S. For this reason, training programs like the Las Vegas Firefighter program are getting national recognition and making a difference in people’s lives. The hands-on only form of CPR is gaining considerable popularity as a viable form of the techniques. Also the public placement of AEDs is also part of the overall push for more CPR resources. Some states are simply pushing CPR training as a requirement for students. In this way, states will produce generations that have the necessary training. In states like Virginia, high school students must become certified to perform CPR before graduating. Other nations are also considering similar mandates. In Denmark, teen drivers cannot obtain a driver’s license until they complete CPR training.
With so many fine approaches to CPR training underway, many hope that more people will survive cardiac arrest episodes. Studies are now underway to determine which programs show the most promise. People can help this national effort, of course, simply by signing up for CPR training in their own communities.
Related articles
]]>CPR training is invaluable for preserving life when catastrophe strikes. It is also finding its way into sporting events. In recent news, various athletes have required CPR. Sometimes it’s an unknown heart condition that leads to a collapse or sometimes it’s pure exhaustion. Whatever the case, bystanders that have CPR training can save the life of an athlete that suffers cardiac arrest. The following news items reflect recent incidents where CPR was performed on the court or field.
Young Wrestler Saved by CPR
Recently a 15-year-old wrestler was the subject of an astounding news story. The teen was dead was seven minutes yet his school principal has just completed CPR training six days before and was able to administer the life-saving techniques until emergency services arrived. The youth had an undetected hypertrophic cardiomyopathy that led to his cardiac arrest; the condition plagues various young athletes though it can be detected through an EKG. The boy’s school did not require the test and the boy was allowed to wrestle. Today he is alive thanks to the timely intervention of his school principal who is certainly gratified that he completed his training!
AEDs and Schools
A young Idaho football player owes his survival to an AED that was placed at his high school. Having collapsed on the field, the boy received CPR from two coaches while a third ran for help and to retrieve the school’s AED. The coaches delivering the CPR are convinced that the boy might never have revived it was not for the AED. They now advocate for these devices which they believe should be placed in all schools as well as other public places.
Teen Girl Saved on Basketball Court
A teen softball player decided to play some basketball for a change at the school gym when she collapsed on the court. The coach ran to her side and knowing CPR, he was able to deliver a couple rounds before others could bring the AED to him. Because she had no pulse, the coach knew to deliver one shock to the girl. He was able to keep her alive until emergency help arrived. Her case was another instance where both CPR and the AED were essential for saving her life that day.
Athletes Do CPR Too!
This past fall a college student athlete was able to help administer CPR before her game. On game days this young woman liked to go to the local coffee shop for a little jolt of caffeine. Upon arriving, she saw a commotion at the entrance where a man had collapsed. Knowing CPR, she was able to help revive him by performing chest compressions until emergency services arrived. In her case, a coffee habit and CPR saved a human life!
Athletics is fun for kids and they can hardly wait to hit the court, track, or their associated venue in order to play their hearts out! Sometimes, their hearts carry an undetected abnormality that stops them in their tracks. Luckily athletic departments now understand the essential need to train in CPR and to keep AEDs on hand. These people were lucky to survive their ordeals and they did because bystanders trained in CPR and were on the scene to help!
]]>