What is CPR?
Cardiopulmonary resuscitation (CPR) is a lifesaving technique useful in many emergencies, including heart attack or near drowning, in which someone’s breathing or heartbeat has stopped.
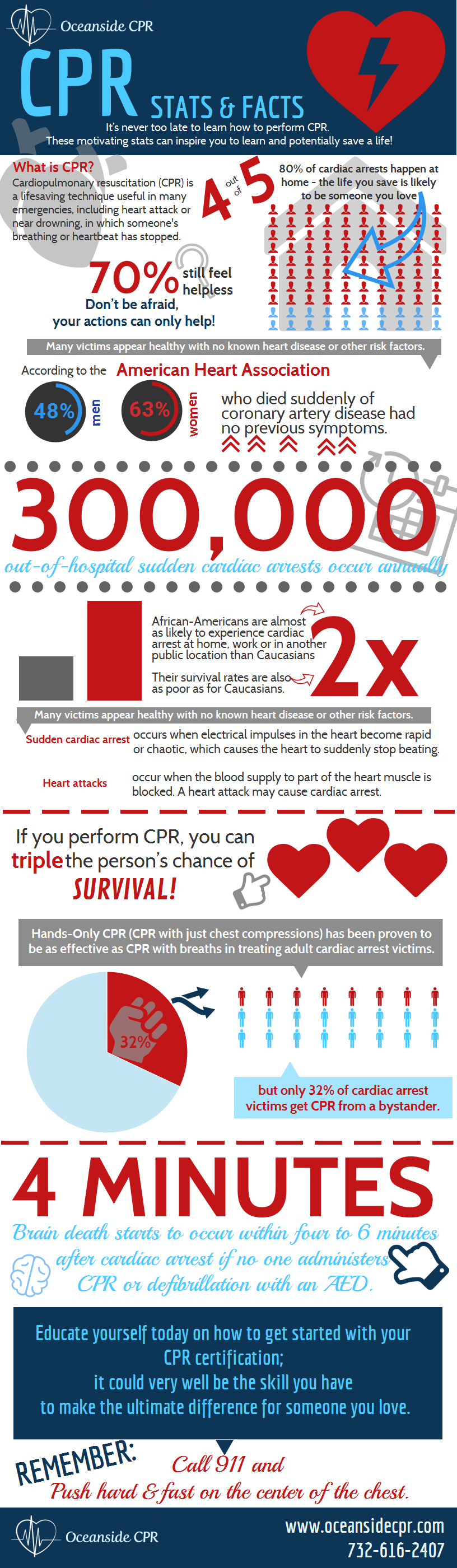
CPR Stats and Facts
Seventy percent of Americans feel helpless -to act during a cardiac emergency because they either do not know how to administer CPR or their training has significantly lapsed. Educate yourself today on how to get started with your CPR certification; it could very well be the skill you have to make the ultimate difference to someone you love. Take a look at these stats and then give us a call:
Share This Infographic On Your Site
- Nearly 300,000 out-of-hospital sudden cardiac arrests occur annually
- Many victims appear healthy with no known heart disease or other risk factors.
- African-Americans are almost twice as likely to experience cardiac arrest at home, work or in another public location than Caucasians, and their survival rates are twice as poor as for Caucasians.
- Sudden cardiac arrest is not the same as a heart attack.
- Sudden cardiac arrest occurs when electrical impulses in the heart become rapid or chaotic, which causes the heart to suddenly stop beating.
- A heart attack occurs when the blood supply to part of the heart muscle is blocked. A heart attack may cause cardiac arrest.
- Effective bystander CPR provided immediately after sudden cardiac arrest can double or triple a victim’s chance of survival
- If you perform CPR, you can triple the person’s chance of survival
- but only 32% of cardiac arrest victims get CPR from a bystander.
- Hands-Only CPR (CPR with just chest compressions) has been proven to be as effective as CPR with breaths in treating adult cardiac arrest victims.
- Brain death starts to occur within four to 6 minutes after cardiac arrest if no one administers CPR or defibrillation with an AED does not occur during that time.
- Less than 8% of people who suffer cardiac arrest outside the hospital survive.
Don’t be afraid, your actions can only help!
If you see an unresponsive adult who is not breathing or not breathing normally, call 911 and push hard and fast on the center of the chest. Anyone can learn CPR – and everyone should!
CPR AED Training Classes At Oceanside CPR
Consider taking a CPR AED training class at Oceanside CPR . Our program is an excellent choice for both the community and workplace and teaches skills with research-proven Practice-While-Watching (PWW) technique, which allows instructors to observe the students, provide feedback and guide the students’ learning of skills.
As CPR instructors with over 25 years of experience, we are able to provide a relaxed and comfortable teaching environment, no matter what class you are looking for. Our goal is to prepare people with the confidence so they can perform CPR in any life-threatening emergency – Without Hesitation! Whether you are interested in attending a class, scheduling an on-site training or just have a general question, please don’t hesitate to contact us at (732) 616-2407.
]]>There are many different situations when CPR can potentially save a person’s life or minimize brain damage and other health problems. Though use of CPR is not always enough to guarantee a person’s survival, when used correctly, it can dramatically increase their chances. CPR training in NJ can help you learn how to identify these life-threatening situations and how to immediately respond. With CPR training in NJ, you’ll have to tools to potentially save the life of a friend, coworker, family member, or stranger.
Situations to Use CPR
When you see someone unconscious or collapsed on the ground, they may need CPR and other forms of assistance. CPR, also known as cardio pulmonary resuscitation, can help restore breathing and beating of the person’s heart and save their life. Individuals who complete AED and CPR training in NJ are better prepared to identify people who might need this type of help.
Some situations that may require CPR include drowning, suffocation, heart attack, allergic reaction, choking, and electric shock. One of the most common situations when CPR is needed is during sudden cardiac arrest. This occurs when a person’s heart suddenly stops beating. This is why it’s so important to check breathing and heartbeat when you encounter someone who looks unconscious.
Cardiac arrest typically happens after a person experiences an especially long or severe type of heart arrhythmia, which is when the heart beats in an irregular rhythm or too slowly or quickly. Anyone could have minor cases of arrhythmia, but some people experience arrhythmia more often or have more serious cases of arrhythmia, and this makes sudden cardiac arrest more likely. Some common causes of arrhythmia include:
Coronary Heart Disease
If you have coronary heart disease, your arteries slowly clog with cholesterol and other deposits. This reduces the amount of blood that can flow to your heart and affects the ability of your heart to beat at a proper rhythm.
Heart Attack
During a heart attack, a person may experience ventricular fibrillation, which is when the lower chambers of the heart wither but do not contract effectively. This is one of the most common causes of heart attacks and one of the most common reasons why people need CPR or AED. CPR training in NJ can teach you how to recognize when this is happening and help you provide treatment quickly and correctly.
Congenital Heart Disease
Some people are born with abnormalities in their heart, and this can make the risk of heart attack and arrhythmia higher. This can even affect adolescents and children and cause them to experience sudden cardiac arrest. When providing CPR to younger victims, it’s very important that the person understand what they are doing. Courses that provide CPR training in NJ teach participants how to provide CPR to different ages, so that you are always prepared during an emergency.
Problems With the Electrical System
Every person’s heart is controlled by electrical signals. These electrical signals tell the heart when to contract, how fast to contract, and how much to contract. When the electrical system is working correctly, the heart beats a normal rhythm, but sometimes the electrical systems stops working the way it’s supposed to. These types of problems are known as primary heart abnormalities. Though rare, there are some conditions that can cause these types of abnormalities such as long QT syndrome and Brugada’s syndrome.
These are only a few of the possible causes of arrhythmia and sudden cardiac arrest. There are many different reasons why a person may suddenly require medical attention, and that’s why CPR training in NJ is so important. Contact us to learn more about our programs and services.
Sources:
http://www.mayoclinic.org/diseases-conditions/sudden-cardiac-arrest/basics/causes/con-20042982
]]>You’ve probably seen defibrillators used on dozens of medical TV shows and in movies. A doctor or medical professional will yell, “Clear!” and a powerful jolt of electricity brings the person magically back to life. Have you ever actually wondered how the defibrillator works and why a jolt of electricity can restore someone’s heartbeat? Though television can sometimes make it seem as simple as jump – starting a car, a defibrillator is a very advanced piece of technology and training can make operating it much easier.
Fortunately, many corporate onsite CPR training courses provide first aid and AED training in addition to CPR training. Learning more about AED technology can help you better understand when you can use it to save someone’s life, and in combination with corporate onsite CPR training, you’ll have the preparation you need to respond during an emergency.
The Electrical System of the Heart
Though it may sound strange, every person’s heart is controlled by electrical signals within their body. Most organs are controlled by electrical signals that are sent through the nervous system from the brain, but the heart actually has its own source of electrical signals. These electrical signals spread from the top of the heart to the bottom and make the muscles in the heart contract. The rhythm of this contraction, also known as the heartbeat, pumps blood throughout the body at a steady rate.
Without constant pumping of blood, a person’s organs and brain won’t receive the oxygen they need and will start to fail. When a person’s heart stops beating, it is called sudden cardiac arrest, and this is when an AED, or automated external defibrillator, can save a person’s life. With corporate onsite CPR training, you will be able to identify these situations and respond immediately to increase the person’s chance of survival. According to some studies, using an AED and performing CPR can double a person’s chance to survive.
Irregular Heart Rhythms
Why does sudden cardiac arrest occur? Though most people’s hearts have electrical systems that work correctly, some people’s hearts do not receive the right type of electrical signals. This affects the rhythm and rate of their contractions and makes sudden cardiac arrest more likely.
Heart rhythms that are not normal are called arrhythmias. Ventricular fibrillation is a common type of arrhythmia that causes the bottom of the heart to beat irregularly. Ventricular tachycardia is another type of arrhythmia affecting the chambers in the bottom of the heart, and both of these arrhythmias can cause sudden cardiac arrest. Arrhythmias can occur in all types of people, and many are not even aware that something is wrong with their heart. Completing corporate onsite CPR training can prepare you for when these emergencies occur unexpectedly.
Using an AED
When someone is experiencing sudden cardiac arrest, an AED might be able to save their life. The electrical signal sent by the device can get the heart beating at the right rhythm again. With its built-in computer, an AED can measure a person’s heartbeat, or lack thereof, and determine if an electric shock is needed. The device’s computer will also be able to determine what type of electric shock is necessary and give instructions so that it’s used correctly.
During this type of emergency, corporate onsite CPR training can ensure that someone knows how to respond and can respond immediately. Every second counts, so it’s important to have people who are trained and prepared. Using an AED correctly can increase a person’s chance of survival to 75%. If you are interested in learning more about AEDs and corporate onsite CPR training, contact us today.
Sources:
http://www.nhlbi.nih.gov/health/health-topics/topics/aed
http://heartsine.com/2012/12/how-does-an-automated-external-defibrillator-work/
]]>
Take the CPR Classroom to You
As a full-service New Jersey CPR class safety company, Oceanside CPR conveniently offers complete BLS (Basic Life Saving) techniques and first aid for company of all sizes. We come to you…on your schedule. Learn emergency preparedness in a fun, fast paced environment and even enjoy a discounted rate per person for group classes!
Be a Lifesaver
Whether you need your CPR/AED course completion card to meet a specific job requirement or you’re a healthcare professional who needs to know how to perform CPR in a hospital setting, our courses are designed to give you the confidence to recognize and act on several life threatening emergencies in a safe, timely and effective manner. It’s difficult to predict where and when a sudden cardiac arrest will occur; however, studies have identified other out-of-hospital high-incident locations including airports, community centers, sports complexes, schools, doctors’ offices, public transportation terminals, gyms, jails, and malls. So, no matter where you are or where you work, having CPR knowledge and skills can literally be a lifesaver.
You Choose the Class
Choose the classes that fit your company’s needs most including: CPR and AED training, AHA BLS for healthcare professionals, pediatric CPR and first aid, basic first aid, and/or babysitting safety. We’ll provide everything needed for the on-site CPR class including CPR manikins, AED trainers and face shields. All of our CPR instructors are on-time, professional, friendly and efficient (plus we offer more than 25 years of certified experience).
Don’t Hesitate- Recertify
The American Heart Association recommends a bi-annual CPR class with an actual CPR recertification every 2 years. The practice behind the best way to administer CPR is always being researched and improved, so while the basics of CPR will remain the same, you’ll gain new knowledge with a CPR recertification.
Get Certified with Private On-Site Oceanside Group CPR Classes in New Jersey
Studies show that starting CPR and using an AED saves lives. Once the heart stops beating, every moment is critical. Find out more about scheduling a private group CPR training class for your company or organization today.
]]>I want to get a certification. That’s it!
Well, a large number of people want to enroll for CPR classes only for the sake of a certification. Most hospitals and healthcare organizations require their employees to have basic knowledge regarding First-Aid, CPR and AED. A person looking for a certification to just get employment in such organizations, has endless options of classes to choose from.
A simple “CPR class” search on Google will fetch a long list of agencies and a variety of training classes for enrollment. However an overwhelming majority of these online agencies have absolutely no standards in granting a certification. They are there to just make money. These agencies may provide a handbook on CPR and conduct an online test before granting a certification. As a matter of fact, a large number of them just hand over a certification for simply registering for the course and paying the fees.
Nonetheless, whether the employing organization will accept the certification from a particular online agency or not is completely at their discretion. Therefore, it is better to know which certifications they accept beforehand, if possible.
I want to learn to administer CPR
It is impossible to learn CPR without some actual practice in the presence of an instructor. The actual practice is done on a mannequin in a CPR class. Only some agencies go to the lengths of providing a mannequin and an experienced instructor to train the students. When I say experienced instructor, he should be someone who has had hands-on experience of administering a CPR. Having someone who has worked as a paramedic or a nurse is the best bet. Likewise, the classes which require their students to demonstrate competence in CPR administration, for awarding a certification are trustworthy.
Various hospitals and EMS providers conduct weekend CPR classes, which are, more often than not, quite good too. But, generally they do not offer certifications for attending their classes.
Remember to ask these questions before enrolling for a CPR class.
- Is hands-on training available?
- Is there a mannequin available on which you can perform chest compressions? Will each student get one to practice?
- Is the instructor experienced?
- What was the nature of his previous job? Did he have the opportunity to perform CPR?
- How rigorous is the training?
- Are there any tests for awarding the certification at the end of the training?
I want to learn as well as get a CPR certification
The certifications awarded by various CPR classes are not valid universally. Whether a certification is considered valid is purely at the discretion of the person and/or the organization asking for it. Overall, there are only 2 organizations whose certifications are widely, if not universally, accepted. They are American Heart Association and American Red Cross. These organizations are known for their excellent training programs. On the other hand, depending on your location, they may not have year-round classes. It is therefore recommended to check for their class schedules in advance.
]]>- No practical Exposure
Let me be blunt about this. You are not competent enough to administer a CPR unless you have practiced it on a mannequin in a live class with an instructor monitoring your actions. Despite of this, the online agencies offer nothing more than some reading material on CPR and a test for awarding a certification. As a matter of fact, most agencies do not even conduct the test and when they do, it is only a formality and has no bearing on your being awarded a certification. There is absolutely no learning involved in the online CPR certifications that would help you in a real-life situation.
- Absence of a Regulatory Norm
There is no dedicated government body to oversee the operations and certifications awarded by the various CPR training agencies. All the agencies, whether online or traditional, have their own approaches. They have their own course material and practice guidelines. Although American Heart Association releases updated CPR guidelines, it is up to the agencies whether to adapt the latest guidelines or continue with the older procedure. American Heart Association and American Red Cross are two of the most trusted agencies which offer reliable online certification programs. Granted, these organizations have online training programs, but they too mandate in-person skills assessment to award the certification.
- Certification Acceptance issues
If you are looking to get an easy certification to fulfill a job requirement, be wary of the online certifications. The acceptance of a certification from a particular agency is solely at the discretion of the employer. If the employer feels the online agency is not qualified or credible enough to grant a certification, then the certification has no weight to it. This is especially true in case of obscure online agencies with no practical training involved.
- Complications of CPR
About 330,000 cardiac arrests happen every year in U.S. alone. A majority of them are at home. That is to say that, an overwhelming majority of people suffer cardiac arrests at home in the presence of other people. The people present at the location during such an emergency, could be the only hope of survival for the victim. A good CPR can considerably improve the chances of the patient’s survival. If the person giving CPR is not well versed with the technique and only knows theoretical concepts from the course material provided by an online certification agency, the victim`s chances of survival are greatly reduced. A badly administered CPR may leave the patient with broken ribs, lung contusion, heart contusion or other injuries.
Whether you wish to learn a lifesaving skill or get the certification to land a job, it is paramount that you enroll for a traditional classroom CPR training class.
]]>1. Am I allowed to do a CPR if I have do not have a certification or never attended any CPR class?
Yes. CPR certification or class training is not mandatory for you to spring to action and extend your valuable help to save a fellow human being`s life. However, some country laws require you to ask for victim`s permission before you perform a CPR on them. CPR classes make you aware of such legal obligations to be mindful of, in the event of such emergencies.
2. Am I obligated to perform a CPR on a victim in emergency, if I am CPR certified?
Except in the state of Vermont, there is no legal obligation in the U.S. for a fellow-citizen to administer a CPR on an emergency victim. The state of Vermont has the Good Samaritan Law (Duty to Aid the Endangered Act), which puts an obligation to a fellow-citizen present in an emergency to extend all the reasonable help that could be provided to the victim. This includes a CPR as well. However, the case is different for professional rescuers such as a firefighters, EMS’s, lifeguards and so on, for whom it is a duty to perform CPR on the victim, if required.
3. Is it better to join a traditional classroom CPR class or an online CPR class?
There is no better way to learn the lifesaving skills than practicing them live on a mannequin. The experience of practicing while being continuously monitored and advised by an instructor is the best method to learn the procedure. Online classes neither offer the depth of knowledge nor the experience that is characteristic of traditional CPR classes.
4. How often do I need to take CPR classes to remain competent in administering a CPR?
With advances in medical science, our understanding of CPR and its effects improve continuously. The CPR guidelines are updated regularly to reflect these changes. In order to keep yourself updated to the latest guidelines and to have enough practice on a regular basis, it is generally recommended to retake the certification every 12 months or less.
5. Are online CPR certifications valid?
Since there is no national level regulatory body to monitor the activities of various CPR training agencies, a number of online CPR certification agencies have cropped up. Their standards for awarding a certification are very low and therefore, it is entirely up to the employer to consider or reject the certification from an online agency.
6. Are the CPR classes different for amateurs and professionals?
Yes. A professional agency such as the American Heart Association has customized training programs for amateurs learning to become capable of saving a loved one in emergency and for professionals such as a daycare provider or a nurse. On a broad level, the CPR classes train students in administering CPR on adults, children and infants. While amateurs are generally trained to provide CPR to adults, the professionals are trained based on their professional requirements.
7. Do I need to pass an examination or a test to get a CPR certification?
All good CPR training agencies require their students to pass a skills test, during which they are required to demonstrate their CPR administration skills in practice. Depending on their performance in the test, they are awarded a certification. Even the well-known CPR training agencies which offer online programs, require the students to perform a physical skills demonstration to award a certification. Nevertheless, many agencies give away certifications without conducting any test and when the tests are conducted, the students are hardly rejected.
]]>As you’ll read in multiple other sections of this supplement, we continue to discern insights into more effective treatment approaches to out-of-hospital sudden cardiac arrest. In reality, we’ve collectively learned more in just the last decade than ever before about the pathophysiology of cardiac arrest.
With considerations about cooling (therapeutic hypothermia), chest compression continuity and alternative ventilation strategies, is there really much to talk about when it comes to something as simple as the rate of chest compressions?
“So, Dr. G, what’s your interest in chest compression rate? The American Heart Association (AHA) says to compress the cardiac arrest victim’s chest at least 100 times a minute. That’s all there is to it, right?”
That’s a good place to start and an understandable question. For purposes of this particular conversation, let’s discuss victims who are of adult age. You’re correct in your interpretation of the AHA guidelines released in late 2010.1 How the 2015 guidelines on chest compression rate will change, if at all, is unknown.
There’s been some interesting science published regarding chest compression rates since those 2010 guidelines.2,3 I’m quite sure the clinicians and scientists charged with formulating those 2015 guidelines will certainly take such discoveries into account. The fact is — no surprise here, I think — nothing is very simple when it comes to a condition as dynamic, dramatic and challenging as cardiac arrest.
Key among the latest scientific papers on chest compression rate is work done by Dr. Ahamed Idris and his colleagues in the Resuscitation Outcomes Consortium. In short, Dr. Idris and the research team found that exactly 100 chest compressions per minute didn’t produce the highest number of survivors among the large group of cardiac arrest victims who were treated by systems that participate in the ROC.4
The “sweet spot” of chest compression rate in that review, published in 2012, was much nearer to 120 chest compressions per minute.4 So, you might say that the AHA is still right because 120 compressions per minute fits the definition of “at least 100 times a minute,” although so does 140 compressions per minute, correct?
“The patients (and their families) we treat often think more is better, and if we want to be honest, many EMTs and paramedics subscribe to that belief about a lot of interventions. That said, I bet you’re getting ready to burst that bubble and tell us 140 compressions per minute may not be better?”
Actually, I’m not going to say 140 compressions per minute may not be better than a rate of 120. Instead, I’m going to say, based upon the Idris paper, that 140 compressions per minute are definitely not better for survival than 120. In that report, a very compelling graph is presented that I choose to describe as a “wave of survival per compression rates.”
The reason I call it a “wave” is that a curve implies an even rise and fall and this isn’t that. The scientific term for the actual curvilinear shape is a cubic spline model, but that’s hard for a guy like me to immediately grasp. I can visualize a wave that rises and then fades out, and I think most people can as well.
So back to that study, it’s not too hard to imagine that survival proved lower at rates less than 100 compressions per minute and then there is a slow increase to a peak in survival near 120 compressions per minute.
Here’s my key point: After 125 and towards 140 and beyond, the survival line drops off! That’s why this study is so important in my opinion, and I trust the researchers, their method of study, plus the number of patients involved was large. This is science you and I can use in our quest to produce more neurologically intact survivors from out of hospital sudden cardiac arrest.
“Why do you think 140 isn’t better than 120? Besides, are people in real life compressing at 140 anyway? That seems pretty fast and not what’s taught in the first place.”
Let me break that up into two answers. First, we have to think about this amazing organism that is the human body. What happens when you and I decide we’re going to get our particular organisms in better shape and do some aerobic conditioning or weightlifting? Why does our heart rate rise and breathing increase? We are doing the “Magic C” as I call it — compensating!
That workout-induced tachycardia and tachypnea is getting greater-than-usual oxygen-enriched blood flow to muscles that require it to perform what we’re asking of them. As long as we are pulsatile, and your patient is pulsatile, our human bodies will stretch compensation to impressive levels. But, what happens when pulsatile becomes pulseless? Compensation ceases, at least the intrinsic compensation.
So what’s the extrinsic compensation during CPR? You. Me. Your partner(s). Bystander(s). CPR is, in one word, compensation.
What percent of compensation do you and I have to attain for a person when we do CPR? 100%! Sobering, huh? We don’t even get to outsource 1%; that 100% needs to be the very best it can be, at least according to the best understanding of what works today.
As important as each compression is, the decompression phase is just as important because that’s when intrathoracic pressure drops and blood flow can return to the heart to be available for flow from the heart on the next compression. Think about the last sick patient you had in a true tachydysrhythmia with a pulse? Why were they so weak, hypotensive and likely even hypoxic? The rapidity of their pulse prevented good cardiac output and perfusion, both to central and peripheral circulation.
We may not be so worried about peripheral perfusion in cardiac arrest, but if our compressions are going to produce helpful cerebral and coronary perfusion pressures, we have to let enough decompression time occur. That doesn’t happen if we compress at 140 times a minute.
So do professionally trained EMTs and paramedics compress that fast anyway? Actually, yes, a lot do. Good – hearted, enthusiastic police officers, firefighters, EMTs and paramedics perform too many compressions. How do I know this? Back in 2011, we discovered in the process of reviewing chest compression fundamentals with each and every EMT and paramedic in the EMS System for Metropolitan Oklahoma City and Tulsa, that without a metronome to guide compressions, nearly 90% of these incredibly well-trained men and women were compressing somewhere between 135–145 times per minute!
That really opened my eyes. It affirmed to me several things: 1) We have EMS professionals in our system who really care about — and work hard at — treating cardiac arrest. Even in training scenarios, their adrenaline kicks in and they go after it! I had honestly thought if we did start using metronomes set at 120 beeps per minute, directly influenced by that ROC study we’ve been talking about, those metronomes would be needed to speed up the rates. But, I was wrong. The reverse was true; we were compressing too fast and the metronomes would help us to slow down.
It became crystal clear to me we needed to begin using metronomes to change natural compression rate tendencies. This turned out to not just be a positive for the patients, but our crews also, because we were actually able to reduce the physical work necessary in performing optimal manual chest compressions.
“Cool, Dr. G. So just compress at 120 a minute in adults, use metronomes set to that and that’s all there is to it?”
Even with what we’ve discussed so far, there’s more to it. To prove the point, I’ll share with you now that we recently changed our compression rate guideline, and metronomes, to 110 compressions per minute in rate.
“What?!?! How does that make sense based upon what we’ve been talking about?”
Back to the “nothing is really simple when it comes to cardiac arrest” mindset. In our particular system, we currently don’t use mechanical chest compression devices like the Physio-Control LUCAS 2 chest compression system or ZOLL AutoPulse non-invasive cardiac support pump. We use a team dynamic plan for coordinated resuscitation (aka the “pit crew” approach). The most common resuscitation in metro Oklahoma City or Tulsa has 5–8 EMS professionals on scene within 4–10 minutes.
In addition, one of the devices we choose to use in our airway management and cardiac arrest care is the ResQPOD impedance threshold device (ITD) for its capability of reducing intrathoracic pressure during decompression — another important factor in cardiac arrest resuscitation.
Further, because of the emphasis we’ve been placing on the continuity of chest compressions and getting quick feedback to our colleagues about how consistent in rates and continuity that their compressions were or were not in individual resuscitations, we’ve seen our chest compression fraction (time of resuscitation in which chest compressions are occurring) move from a typical 85% to more than 95%.
Without getting too far down in the weeds of science, it’s important to point out that use of mechanical chest compressors and/or the impedance threshold device can influence the basic physiology of hemodynamics produced by compressions.
Through very in-depth conversations that I’ve had over the past few years with the clinical scientists who developed the impedance threshold device, it appears that the ideal compression rate for CPR without an ITD, as reported in the Idris paper, differs from what’s ideal if an impedance threshold device is used in-line in the airway circuit.
It seems the best rate when using an impedance threshold device is much closer to the 100 compression rate per minute; in fact, in subsequent data analysis, the best overall survival in the ROC study occurred in patients who received an active ITD with chest compression rates close to 100/min. So, we’re slowing down to 110 for now, primarily based upon both this specific data analysis and our system-specific chest compression fraction and effective compressions per minute. We’ll continue to follow our survival outcomes and adjust our chest compressions rates as further observation and science dictates.
To illustrate how complex this can get, if active compression – decompression CPR with an ITD finds its way to the streets of the United States, that ideal chest compression rate may be as low as 80/min according to a recent U.S. study!
It does make sense when you appreciate that all of these things produce different compression types and intrathoracic pressure and, thus, different compression types and adjuncts, like the ResQPOD ITD and mechanical compression devices, will produce different optimal rates.
Just remember, it still is all about survival and there are a lot of “fine tuning” knobs to turn back and forth as science gives us updates to our user’s manual for resuscitation.
“Wait, Dr. G. So you’re talking a lot about rate, but not so much specifically about metronomes. Seems like those are more important than you first thought and if anything, they’re getting even more important. Why don’t the monitor/defibrillators have metronomes adjustable from 100 per minute? Should we ignore those? And, what metronomes should we be buying?”
First, you’re right. Metronomes are far more important than I first thought. In fact, credit goes to paramedics in our system who pushed the concept. I’ll claim to be smart — smart enough to listen to what proved to be their great idea.
Those early metronomes came about because not all the responding companies (fire-based) had manual monitor/defibrillators and not all of our monitor/defibrillators had built-in metronomes at the time. And, for my manufacturing colleagues reading this article, I’ll admit some frustration at the lack of their built-in metronomes being changeable in rate. But, I’ll also admit that I understand the frustration that these manufacturers have themselves because they can’t put a “dial the rate up or down” knob or touchscreen on their devices without a time-intensive and costly journey through the Food and Drug Administration review and approval process.
Should you ignore those metronomes that come with the cardiac monitor/defibrillators? Not if your local medical oversight physician(s) want you to use them. If they do, please use them per your system-specific treatment guidelines.
In our system, we’ve purchased musical metronomes that do allow for rate changes. This made it possible to start at 120 beeps per minute, change to our current 110 beeps per minute, and still allow for future changes. I’m pretty sure these music industry companies have no idea what paramedics are doing ordering dozens of metronomes. They probably think we’ve got some great garage bands in urban Oklahoma!
Many options exist in the marketplace. I recommend you try to find something that’s easy to activate and see or hear, with the durability of the proverbial EMS steel ball, something that allows for rate changes (but doesn’t allow crews to change it to undesired rates or allow unintended changes in rates), and something sized to promote ready accessibility.
There are a lot of smartphone apps with audible and visual metronomes that are adjustable as well. We considered use of smartphone apps, but didn’t want to ask our EMS professionals to use their personally owned devices in the provision of resuscitation.
Many of the agencies in our EMS system have found great ways to physically attach metronomes to the outside of their AEDs or manual monitor/defibrillators so initial arrival EMTs and paramedics don’t have to go fishing in a pocket or compartment to find it in the early and chaotic first minutes of resuscitation. Easy access always promotes consistency in early use.
“So, Dr. G.: What kind of improvement have you seen in resuscitation practices in the EMS System for Metropolitan Oklahoma City and Tulsa since your crews started using these metronomes during cardiac arrest resuscitations?”
We made an assumption when the pit crew protocol was finalized and initially implemented, that the medics were providing 120 compressions per minute per our protocol. All of the involved agencies had metronomes at that time and there was nothing to lead us to believe this rate was in question.
When we participated in a cardiac arrest resuscitation analytics annotation pilot project sponsored by one of our industry partners in February and March of 2014, we found that the compression rates on some cases were alarmingly high while others were at or near 120. So we added a field to the data we collect and the CPR rates have been continuously tracked since that time.
One of the things we found early on was that some of the smaller sized metronomes were not being used for various reasons. In some cases, it was simply because the crews forgot to use them, though in others it was because the Velcro that had been used to attach them to the monitors had become worn and the metronomes either fell off and were lost, or they were simply placed in the monitor case where EMTs and paramedics didn’t know they were relocated. Like they say, out of sight can equal out of mind!
We also learned that environmental noise can cover the sound of the metronome, so, whatever metronome you use, it has to be capable of being heard and/or seen. The metronomes built into the cardiac monitor/defibrillators do seem to solve that problem, but I want to caution that I personally don’t think 100 compressions per minute for all cardiac arrest patients, in all resuscitation practices is the optimal rate as we know it today.
In all of the cases in our specific system when the metronome wasn’t used, the compression rate was certainly faster than the 120/min we desired. Interestingly, when the ambulance would go en route to the hospital, rates often jumped almost immediately from around 120 to 130 and above.
After we mounted a concerted effort to have the providers utilize the metronomes and began revealing the patterns in compression rates at our monthly CQI meetings and additionally in emails to the education departments in our system agencies, we found almost immediate elimination of extreme compression rate deviations (e.g., greater than 160/min).
Our typical rate is now 123/min. Keep in mind we’re still rolling out the change to 110/min. This is down from 129/min. It doesn’t sound like much, but there are nearly 100 workable arrests every month in our system and that’s a great achievement by our fire and EMS crews in focusing on hitting that compression “sweet spot” of compressions per minute. We believe it has strongly contributed in increasing our successful resuscitations.
“Thanks, Dr. G. Do you have any parting thoughts?”
It’s an exciting time in EMS resuscitation. It takes work on everyone’s part to keep pace with the findings we’re putting into practice. Thanks for your commitment to excellence in out-of-hospital EMS medicine by reading this article. Together we’re finding better answers to challenges like cardiac arrest, answers that truly make a life or death difference to people we serve, and when they need those answers most. Keep reading and asking questions because scientific discoveries are happening in EMS medicine now more than ever.
References
1. Field JM, Hazinski MF, Sayre MR, et al. Part 1: Executive summary: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(suppl 3):S640–S656.
2. Field RA, Soar J, Davies RP, et al. The impact of chest compression rates on quality of chest compressions: A manikin study. Resuscitation. 2012;83(3):360–364.
3. Jäntti H, Silfvast T, Turpeinen A, et al. Influence of chest compression rate guidance on the quality of cardiopulmonary resuscitation performed on manikins. Resuscitation. 2009;80(4):453–457.
4. Idris AH, Guffey D, Aufderheide TP, et al. The relationship between chest compression rates and outcomes from cardiac arrest. Circulation. 2012; 125(24):3004–3012.
5. Aufderheide TP, Nichol G, Rea TD, et al. A trial of an impedance threshold device in out-of-hospital cardiac arrest. N Engl J Med. 2011;365(9):798–806.
6. Aufderheide TP, Frascone RJ, Wayne MA, et al. Standard cardiopulmonary resuscitation versus active compression-decompression cardiopulmonary resuscitation with augmentation of negative intrathoracic pressure for out-of-hospital cardiac arrest: A randomized trial. Lancet. 2011;377(9762):271–352.
7. Kern KB, Stickney RE, Gallison L, et al. Metronome improves compression and ventilation rates during CPR on a manikin in a randomized trial. Resuscitation. 2010;81(2):206–210.
Cardiopulmonary resuscitation (CPR) and automated external defibrillators (AED) double, and in some cases triple, a victim’s chances of survival if administered quickly after a cardiac episode. While many people are aware of the CPR principles, few are trained in current methods and even fewer are familiar with AED concepts. The American Heart Association estimates that over half of Americans have never actually seen an AED.
Oceanside CPR, an American Heart Association training site and American Health and Safety Training center, offers current CPR AEDcertification for those with little or no medical background and those seeking to renew certifications. The class topics include alleviating choking and CPR AED techniques for adults, children and infants.
Oceanside’s CPR AED classes incorporate the proven Practice-While-Watching method of learning, allowing students to perform tasks and solve problems as instructors look on and provide feedback. Upon completion of the course, students receive their CPR AED certification card, which remains valid for two years.
While CPR is an effective life-saver, many cardiac incidents involve an arrhythmia that can only be addressed with both CPR and AED methods. Almost a quarter of cardiac arrest victims suffer from these events and can be stabilized with an AED.
Contact us to review the list of class dates, times and locations in and around New Jersey, and help reduce the number of deaths from sudden cardiac arrest.
Related articles
]]>The Silvester Method
The truth is that no single person is responsible for inventing CPR. There have been dozens of procedures over the years which incorporate “parts” of modern-day CPR. The Silvester Method is one such procedure that helped shape modern-day CPR into what it is. Created by Doctor H. R. Silvester in the 19th century, the Silvester Method is characterized by lying the victim down on his or her back, raising their arms, and pressing down onto the chest to trigger exhalations. This is done at a pace of 16 times per minute.
Holger Nielsen
In 1911, the Holger Nielsen method was published in a Boy Scout’s handbook. It’s was strikingly similar to the Silverster method but for one major difference: in the Holger Nielsen method, the victim is placed face-down on the floor or ground, at which point the person performing the procedure pressed against the victim’s back to force air into their lungs. This became a highly popular method, and it was even depicted in an episode of Lassie, as well as several cartoon shows. The concept between the Holger Nielsen and Silvester Method are pretty much the same, with the only difference being the position of the victim.
A Pulse of Life
While these two techniques were widely used at the time, it wasn’t until the mid 1800s when a standardized method involving both chest compressions and mouth ventilations began to form. Three esteemed medical professionals, James Jude, Guy Knickerbocker and Peter Safar, created a video which depicted both of these techniques being used in a single procedure. The video, titled “A Pulse of Life,” gained acceptable in the medical community in the years to follow.
So, why did Jude, Knickerbocker and Safar feel the need to include mouth ventilations into the procedure? They believed that ventilations were necessary to keep the victim’s blood oxygenated. While this helped shape CPR into what it is today, the American Heart Association (AHA) has since debunked this theory, stating that mouth ventilations are not required.
To recap, CPR is the culmination of centuries worth of medical studies and data. While the details have changed, the overall concept remains the same: to keep victims of cardiac arrest alive by promoting blood flow to the heart.
]]>